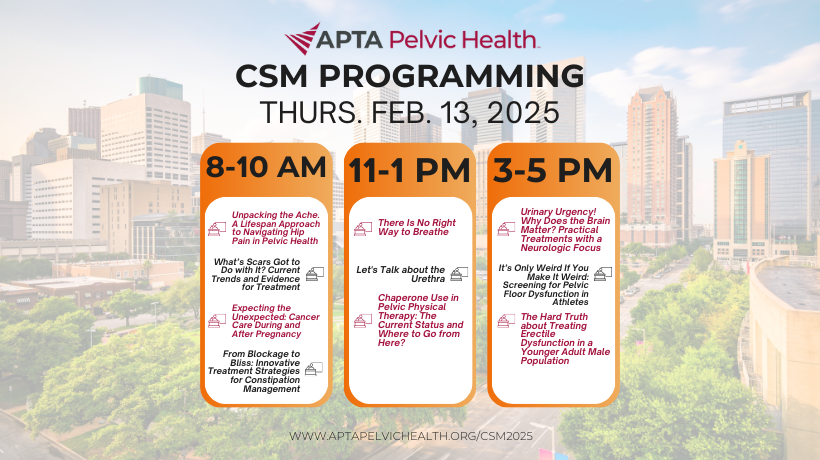
CSM 2025: Day 1 Pelvic Health Programming
Get ready for an exciting start to CSM 2025 with Day 1 programming packed full of dynamic sessions and expert-led discussions! Whether you're diving into the latest in pelvic health research or honing your clinical skills, Day 1 promises to deliver cutting-edge knowledge and networking opportunities you won’t want to miss. Join us to kick off this unforgettable event and take your practice to the next level!
Day 1 Sessions
8:00 AM - 10:00 AM What’s Scars Got to Do with It? Current Trends and Evidence for Treatment
Presented by Elizabeth Geiger Harvey PT, DPT, MSR, Board-Certified Pediatric Clinical Specialist, and Heidi Ewen PhD, FGSA, FAGHE
Wound specialists are critical in managing skin integrity throughout the patient's lifespan. 250 million people acquire surgical wounds or traumatic lacerations annually and up to 70% become pathological. Despite the high rate of comorbidities present with postoperative scars, there is little evidence to demonstrate how physical therapists (PTs) perceive their relevance or manage these types of scars. This course reviews the results of the Postoperative Scar Survey in which almost 1000 PTs participated. PTs' understanding, beliefs, and practices will be reviewed across patient populations and practice settings. Preferred assessment and treatment strategies (i.e., IASTM, taping) used by PTs, as well as perceived barriers to scar treatment will be reviewed.
8:00 AM - 10:00 AM Expecting the Unexpected: Cancer Care During and After Pregnancy
Presented by Alexandra Hill PT, DPT, Board-Certified in Orthopaedics and Women's Health, and Rebeca Segraves PT, DPT
Cancer has become the second most common cause of death among women during reproductive years. Cancer rates during pregnancy are rising, in part due to advanced maternal age, increased rates of obesity, and earlier detection of disease (Arup 2023). Individuals who navigate a cancer diagnosis during pregnancy often face complex physical and mental health challenges throughout their treatment and long-term recovery (Di Mattei 2023). This interactive session will examine the role of physical therapists on interdisciplinary teams during and immediately after pregnancy in the setting of cancer diagnosis and treatment. Speakers and audience members will examine maternal health disparities, physical and mental health concerns, fertility and reproductive considerations, the role of rehabilitation, and the impact of cancer on obstetric health outcomes.
8:00 AM - 10:00 AM Unpacking the Ache. A Lifespan Approach to Navigating Hip Pain in Pelvic Health
Presented by Jennifer Ann LaCross PT, DPT, PhD, ATC, CLT-LANA, Board-Certified Women's Health Clinical Specialist, and Edward Patrick Mulligan PT, DPT, ATC
This session offers a contemporary overview of hip pain conditions throughout the female lifespan, tailored specifically for the pelvic health physical therapist. Attendees will gain insights into clinical identification of bony and soft tissue disorders, with a focus on understanding the hormonal influence on these conditions. The session will explore differential diagnostic strategies, the role and use of imaging, and discuss management perspectives that consider underlying morphology and post-operative technique. The primary focus will emphasize treating hip pain after systemic and local pelvic health contributions have been identified and/or addressed, ensuring a more holistic full-person approach that targets hip-specific symptom drivers. Drawing from the latest evidence-based practices, this session will assist the pelvic health therapist in maximizing treatment outcomes while also recognizing prognostic factors that impact terminal outcome expectations for their patients with hip pain.
11:00 AM - 1:00 PM There Is No Right Way to Breathe
Presented by Iris Platt PT, DPT, and Claire Marie Hamnett PT, DPT, Board-Certified Women's Health Clinical Specialist
Breathing is an essential component in the maintenance of human life. Diaphragmatic breathing (DB) is promoted as the optimal breathing pattern for improving pelvic floor and core function as well as in the treatment of pelvic dysfunction and chronic pain. Where did this idea come from? Are we able to change patients' default breathing patterns? Is DB optimal all the time? What does it mean to manage intraabdominal pressure “correctly”? How does posture, ribcage mobility, and core strength play a role in a patients’ functional capacity? This session will discuss the role of DB as one of many different ways to breathe to promote variability and adaptability in patients with pelvic conditions. In addition, the session will cover examination of DB as well as manual interventions and verbal/tactile cues for physical therapists to use in the clinic.
11:00 AM - 1:00 PM Let's Talk about the Urethra
Presented by Mary Jane Strauhal PT, DPT, BCB-PMD
Urethral symptoms can affect all age groups, all races, and all genders. There are multiple etiologies, and symptoms can co-exist with, be confused with, or be misdiagnosed as conditions with similar presentations, such as interstitial cystitis or prostatitis. Proposed etiologies include pelvic floor dysfunction, sensory dysfunction, dietary factors, environmental factors, infections, inflammation, obstructions, and hormonal imbalances. There is a need to differentiate symptoms, review current diagnostic workups, and consider the various treatment options available to the pelvic health PT. This session will focus on current evidence-based evaluation and treatment of conditions such as urethral pain, urethral syndrome/urethral pain syndrome, dysuria, nocturia, and other symptoms frequently associated with the urethra.
11:00 AM - 1:00 PM Chaperone Use in Pelvic Physical Therapy: The Current Status and Where to Go from Here?
Presented by Mary Austin PT, DPT, Board-Certified Women's Health Clinical Specialist, and Nora O'Leary Arnold PT, DPT, Board-Certified Women's Health Clinical Specialist
The presence of a chaperone for sensitive examinations in medical settings, in particular for vaginal examination and treatment in pelvic physical therapy practice is not currently standardized and has been minimally reported on in the literature to date. Current recommendations by US based medical associations suggest a chaperone be offered to the patient receiving a vaginal exam, but is not required by default. In many practice settings where vaginal exams are performed routinely, the ability to provide a chaperone for every patient encounter requiring a vaginal exam is often limited by staffing and associated financial barriers. This session will review current recommendations and position statements put forth by US based medical associations representing providers who routinely perform vaginal examinations, highlight research that reports on chaperone use from the patient and provider perspective, discuss chaperone definitions and special considerations, and identify benefits of and limitations to chaperone use. A panel discussion of pelvic health physical therapists practicing in a variety of clinical settings will offer their insights on chaperone use to help generate a comprehensive and realistic approach to moving best practices for chaperone use in pelvic physical therapy forward.
3:00 PM - 5:00 PM Urinary Urgency! Why Does the Brain Matter? Practical Treatments with a Neurologic Focus
Presented by Amanda Thompson Mahoney PT, DPT, Board-Certified in Orthopaedics and Women's Health, and Lauren Rachal PT, DPT
In those able to maintain continence, the decision to void is influenced by the strength of the sensation to void and if it is a socially acceptable time and place. The periaqueductal gray and higher brain centers are critical to this executive functioning process. The periaqueductal gray has connections with the thalamus, the prefrontal cortex, anterior cingulate cortex, and insula. Alterations in brain activity have been seen with bladder filling in those impacted by urgency urinary incontinence. During a motor task, attention to urinary urgency reduces those resources available for safe dual task performance. Studies on dual task conditions indicate that urgency has been associated with falls, changes in gait speed, and other spatiotemporal measures. Cognitive training has been used with activities such as urge deference in the overactive bladder population. Dual task training has been impactful in the aging population and in those with neurologic disorders. According to motor learning theories, early learning requires high cognitive demand on higher brain centers. Once the skill is learned, less cognitive focus is required, thus freeing executive function resources for success under dual task conditions. Therefore, individuals with urgency may benefit from directed cognitive focus early, progressing to reduced attentional demand once achieving automaticity with urge deference strategies. The bladder brain connection ideally should be considered when working with patients with lower urinary tract symptoms (LUTS), specifically urinary urgency with or without incontinence. Potential models for DT intervention design will be discussed.
3:00 PM - 5:00 PM It’s Only Weird If You Make It Weird: Screening for Pelvic Floor Dysfunction in Athletes
Presented by Dillon M. Estes SPT, and Ashlie Crewe Campitella PT, DPT, Board-Certified Women's Health Clinical Specialist
An overall prevalence of pelvic floor dysfunction (PFD) is 33% of athletes, including 45% in females and 14.7% in males (Culleon-Quinn, 2022). Aside from the negative physical impacts of PFD, these individuals may also experience embarrassment or anxiety, commencing a domino effect that leads to a decline in athletic performance and overall quality of life. However, screening for PFD is uncommon as a standard practice in screening the athletic population. This session outlines a research project investigating the prevalence of PFD among college-aged athletes, performed by DPT students with minimal training in pelvic floor dysfunction. Based on the results of the project, the researchers posit a simple 2-part protocol aimed at screening athletes of all ages for PFD through noninvasive assessment strategies to determine possible referral to a pelvic health physical therapist. This screening process would allow for early and efficient identification of signs and symptoms of PFD, without intensive training required for the person performing the screen. Once PFD is identified, an appropriate referral to a provider with training in PFD can be made, thus facilitating earlier access to skilled care, which may impact the downstream mental health effects of PFD symptoms in sport as well as allow for optimal physical functioning for the athlete.
3:00 PM - 5:00 PM The Hard Truth about Treating Erectile Dysfunction in a Younger Adult Male Population
Presented by Chad E. Woodard PT, DPT, Board-Certified Sports Clinical Specialist, and Jacob Karl Bartholomy PT, DPT
Sexual and erectile dysfunction are shown in the evidence to increase in prevalence with age, but a younger group of men is also significantly experiencing erectile dysfunction who can be helped by pelvic floor physical therapy. Often this is due to an overactive pelvic floor preventing proper function and contraction of the musculature responsible for erections. This session will describe the relevant pelvic anatomy for proper erectile function, describe medical findings to be ruled out for appropriateness of treatment and patient safety, review the literature to demonstrate prevalence rate and risk factors, as well as apply evidence informed clinical treatments for the improvement of erectile function. The psychological impact of sexual and erectile dysfunction for these men will also be discussed, citing literature and clinical experience. While much of the literature and discussion regarding male pelvic health centers on post-prostatectomy care and the potential for erectile dysfunction following operative intervention, this session will instead focus on men without prostate removal but who are still significantly impacted. Participants will leave this session with an understanding of the relevant pelvic anatomy, apply evidence-based treatment approaches, analyze the mental health implications of this condition, and understand the scope of practice for pelvic health specialists.
Register Now
*Please note that registration for this conference is hosted through the APTA CSM Registration website. You have the option to also register for the full CSM conference or just this specific pre-conference.
Visit the Pelvic Health Booth #2025
Exhibit Hall Unopposed Hours: 10:00 AM - 11:00 AM and 1:00 PM - 3:00 PM
Members, Get Involved: Volunteer at CSM
CSM 2025 Sponsorship Opportunities!
View All Pelvic Health Programming
PT in the Community: Make an Impact During CSM Week in Houston